It's not as simple as saying PTSD causes sleep apnea. The reality is far more tangled—think of it as a feedback loop where each condition feeds the other. The deep-seated effects of trauma can create the perfect storm for sleep-disordered breathing to take hold, kicking off a cycle that’s incredibly hard to break.
The Hidden Connection Between Trauma and Sleep Apnea
For anyone who has experienced trauma, you know the struggle doesn't stop when the lights go out. Post-traumatic stress disorder is notorious for wrecking sleep, with studies revealing that about 70% of individuals face significant sleep issues like insomnia or recurring nightmares.
Breaking that down further, a staggering 41% of people with PTSD report trouble just falling asleep, while nearly half (47%) can't seem to stay asleep through the night. If you're interested in the specifics, you can read the full research about these sleep disturbances to see just how widespread this is.
This constant disruption traps the body in a state of hyperarousal. Imagine your internal alarm system is permanently stuck in the "on" position, always on the lookout for danger. This isn't just a feeling; it’s a physiological reality that wears you down. When your system is constantly flooded with stress hormones, it impacts everything from muscle tension to your heart rate, even when you're supposed to be resting.
A Two-Way Street
The relationship between PTSD and sleep apnea is often bidirectional—a genuine two-way street where each one makes the other worse.
- PTSD Can Increase Sleep Apnea Risk: The chronic stress and hypervigilance that come with PTSD can lead to instability in the upper airway muscles during sleep, making them more likely to collapse.
- Sleep Apnea Can Worsen PTSD Symptoms: The constant awakenings and oxygen drops from sleep apnea fragment your sleep and put even more stress on your body. This can intensify PTSD symptoms like irritability, exhaustion, and emotional dysregulation.
This vicious cycle is precisely why treating only one of the conditions often leads to frustratingly incomplete results. Leaving sleep apnea unaddressed can make PTSD symptoms feel a hundred times worse, while the persistent stress from PTSD creates an environment where sleep-disordered breathing can flourish.
Let's quickly summarize the core connection.
PTSD and Sleep Apnea At a Glance
| Concept | Key Finding |
|---|---|
| Bidirectional Link | PTSD and sleep apnea mutually reinforce each other in a feedback loop. |
| Hyperarousal | A key PTSD symptom that creates physiological stress, making airways unstable. |
| Symptom Amplification | Poor sleep from apnea worsens PTSD symptoms like fatigue and irritability. |
| High Prevalence | Research shows a significantly higher rate of sleep apnea among veterans with PTSD. |
This table just scratches the surface, but it highlights how deeply intertwined these two conditions are.
Understanding how chronic stress torpedoes your rest is the first critical step. The state of high alert from PTSD makes getting deep, restorative sleep feel almost impossible, which only digs the hole of exhaustion deeper. Our guide on how hitting snooze can help reduce chronic stress offers more on this dynamic.
In the sections ahead, we’ll continue to untangle this complex relationship, offering clear answers and practical steps you can take.
Getting to Grips with Each Condition

To really understand how post-traumatic stress disorder (PTSD) and sleep apnea are intertwined, it helps to break them down one by one. It's like trying to solve a puzzle—you have to look at each piece separately before you can see how they fit together to create the bigger picture.
What Is Post-Traumatic Stress Disorder?
At its heart, PTSD is the body's survival instinct stuck in overdrive. After someone goes through a traumatic event, the brain's natural "alarm system"—that fight-or-flight response—can get jammed in the 'on' position. Imagine you’re constantly on lookout for a danger that has long since passed.
This state is called hypervigilance, and it’s a hallmark of PTSD. It leaves you feeling constantly on edge, jumpy, and unable to truly relax. This isn't just in your head; it’s a full-body experience. Stress hormones like cortisol and adrenaline flood your system, keeping your body on high alert and throwing nearly everything out of whack, especially sleep.
The symptoms of PTSD usually show up in a few distinct ways:
- Re-experiencing: This is when the trauma feels like it's happening all over again through intrusive memories, vivid nightmares, or flashbacks.
- Avoidance: Someone might actively stay away from people, places, or even thoughts that remind them of what happened.
- Negative Mood and Thoughts: This can manifest as ongoing feelings of fear, anger, and guilt, or a sense of emotional numbness and detachment from others.
- Changes in Arousal and Reactivity: This is that hypervigilance in action—being easily startled, having trouble concentrating, or experiencing angry outbursts.
Ultimately, PTSD traps the mind and body in a constant defensive crouch, making genuine rest and recovery feel almost impossible.
What Is Obstructive Sleep Apnea?
Now, let's look at Obstructive Sleep Apnea (OSA). A good way to think about it is to imagine your airway as a soft, flexible straw. While you're awake, the muscles around it keep it wide open. But when you drift off to sleep, those same throat muscles naturally relax.
For someone with OSA, those muscles relax a bit too much. This causes the "straw" to narrow or collapse entirely, cutting off your breath for anywhere from a few seconds to over a minute.
Your brain, sensing the emergency of plummeting oxygen levels, sends a panic signal. It jolts you just awake enough to tighten those muscles and gasp for air. This is often what causes the loud snorts, gasps, or choking sounds that partners of people with sleep apnea know all too well.
This is so much more than just snoring. It’s a vicious cycle of suffocating and waking up—a cycle that can repeat hundreds of times every single night. Most people have no memory of it, yet it completely wrecks their ability to get restorative sleep.
This endless disruption means you never reach the deep stages of sleep your body and brain need to repair themselves. The fallout is what you feel the next day: profound exhaustion, brain fog, and a massive strain on your heart and overall health.
Once you understand these two pieces, it starts to make a lot more sense how a mind stuck on high alert from PTSD could easily set the stage for a physically unstable airway at night.
How Trauma Physically Changes Your Breathing During Sleep
It seems strange, right? How can a psychological wound from trauma cause a physical breathing problem while you sleep? The answer is buried deep in your body's wiring, specifically in the chronic stress response that PTSD kicks into permanent overdrive.
Think of your body like a car. Normally, you press the gas when you need to go and hit the brakes when you need to stop. But with PTSD, it's as if the accelerator is stuck to the floor, 24/7. This constant "fight or flight" state redlines every system, leading to very real, physical changes that mess with your breathing.
The command center for all this is your autonomic nervous system (ANS). This is the silent operator managing all the things you don't consciously control—your heartbeat, digestion, and, most importantly here, your breathing. PTSD throws this entire system into chaos.
The Autonomic Nervous System on High Alert
Your ANS is a beautifully balanced system with two opposing parts:
- The Sympathetic Nervous System (The Gas Pedal): This is your "fight or flight" trigger. It floods your body with adrenaline, jacks up your heart rate, and gets you ready to face a threat.
- The Parasympathetic Nervous System (The Brake Pedal): This is your "rest and digest" mode. It slows everything down, promoting calm, recovery, and deep sleep.
In someone with PTSD, the gas pedal is always being pushed, while the brake is weak and unresponsive. Your body is constantly braced for danger, even when you’re tucked into bed. This state of relentless hyperarousal is a core reason why sleep apnea so often goes hand-in-hand with PTSD.
This non-stop alert status has a direct effect on the soft, delicate muscles in your upper airway. When you fall asleep, those muscles are supposed to relax. But in a body swimming in stress hormones like cortisol, that relaxation is anything but smooth. The muscles can become erratically tense or, conversely, too limp, disrupting the open, stable airway you need to breathe easily.
An airway in a chronically stressed body is like a tent in a windstorm. The constant buffeting from stress hormones and an overactive nervous system makes the structure weak and prone to collapsing at any moment.
How Stress Hormones Weaken the Airway
That constant flow of cortisol and adrenaline does more than just make you feel on edge. These hormones directly impact muscle tone all over your body, including the crucial pharyngeal muscles responsible for keeping your airway open. Over time, this chronic chemical stress can lead to inflammation and poor neuromuscular control, essentially making the airway "floppier" and much more likely to collapse during sleep.
This isn't just a theory; we can see it in the data. A groundbreaking study involving twins really drove this point home. Researchers found that the twin with a PTSD diagnosis had significantly more breathing interruptions than their sibling without it. They experienced an adjusted increase of 10.5 events per hour, making it clear that the trauma itself—not just shared genetics—was the driving factor. You can dive into the detailed findings of this twin study to see just how direct the connection is.
Decoding The Overlapping Symptoms Of PTSD And Sleep Apnea
If you're feeling perpetually exhausted, irritable, and can’t seem to focus, you're not alone. Many people with PTSD struggle with these exact issues every single day. But here's the catch: those same symptoms are also classic red flags for obstructive sleep apnea (OSA), which creates a confusing overlap that can easily hide the real problem.
This symptom mimicry is one of the biggest challenges in getting a correct diagnosis. A doctor might see a veteran's crushing daytime fatigue and assume it's just part of their PTSD, completely missing the fact that their body is being starved of oxygen all night long. This often leads to treatment plans that only address half of what's really going on.
Learning to recognize this overlap is the first and most critical step toward advocating for yourself and finally getting the comprehensive care you need.
Spotting The Difference
While many symptoms can blur the lines between PTSD and sleep apnea, there are a few key clues that can help point you and your doctor in the right direction. It's all about looking for the unique signatures that each condition leaves behind.
- Distinctly PTSD: Some experiences are unique to post-traumatic stress. These include things like flashbacks, intrusive and unwanted memories, and actively avoiding people or places that remind you of the trauma. These are psychological responses directly wired to the past event.
- Distinctly Sleep Apnea: On the other hand, some signs are purely physical. Loud, chronic snoring is a big one. So are witnessed pauses in breathing during sleep (often noticed by a partner), or waking up suddenly, gasping for air. These are tell-tale signs of a physical airway blockage. If snoring is a problem, our guide on how to stop snoring naturally might offer some helpful tips.
This infographic really puts the connection into perspective, showing just how much more common sleep apnea is for those with PTSD.
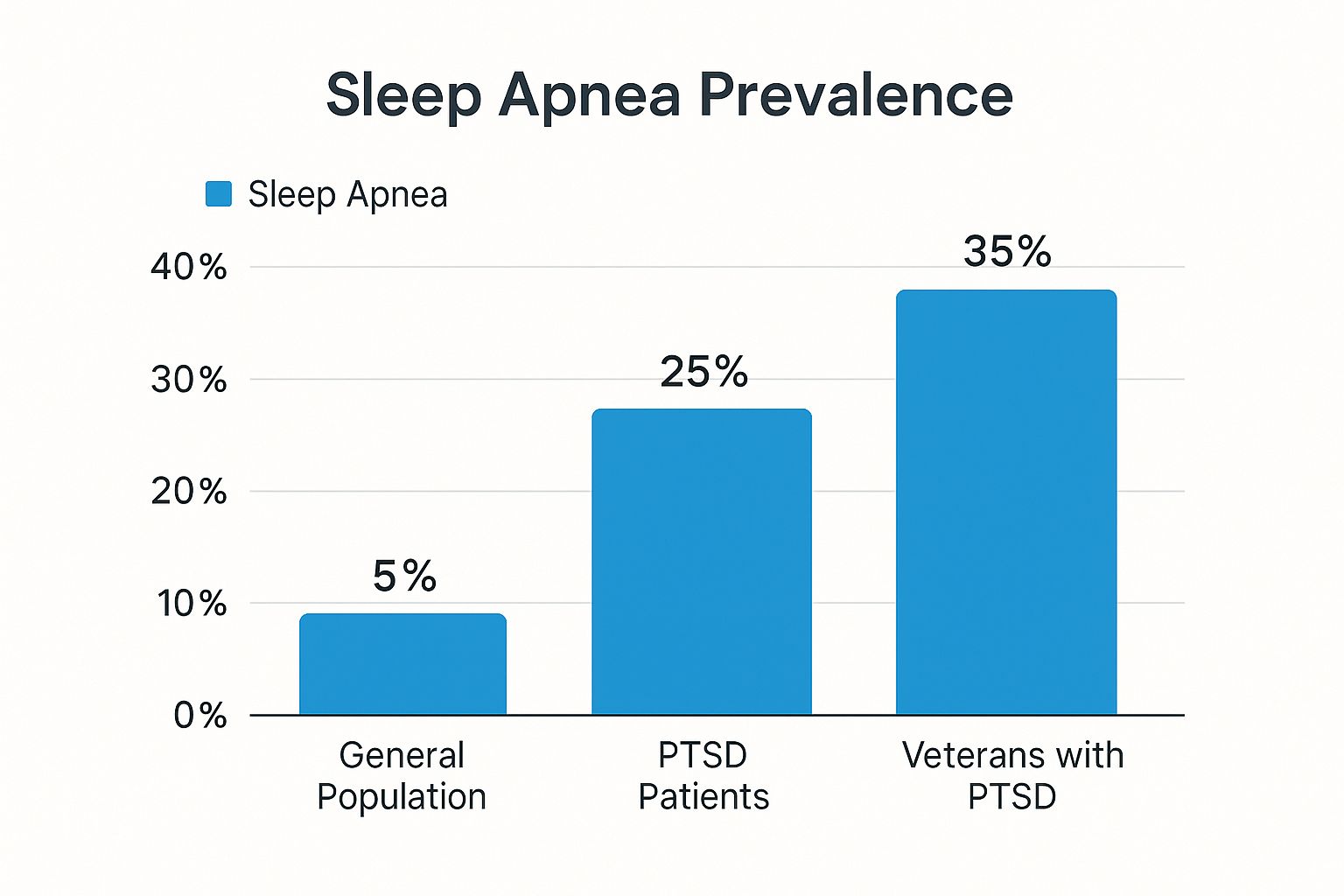
The numbers don't lie. Having PTSD significantly increases your risk for sleep apnea, which is why it's so important to screen for both conditions, not just one.
The link is incredibly strong. Some studies have found that up to 69% of veterans with PTSD also screen as high-risk for obstructive sleep apnea—a rate that dwarfs that of the general population. One major piece of research on veterans from Iraq and Afghanistan found that a staggering 69.2% were at high risk for OSA, and that was even after adjusting for common risk factors like age and weight. You can read more about these groundbreaking findings here.
Symptom Overlap PTSD vs Sleep Apnea
To make things clearer, let's break down how these symptoms can look side-by-side. It can be tough to untangle them on your own, but seeing the differences laid out can be a real eye-opener.
| Symptom | Common in PTSD? | Common in Sleep Apnea? | Key Differentiator |
|---|---|---|---|
| Daytime Fatigue | Yes | Yes | Sleep apnea fatigue feels like profound physical exhaustion, even after a full night's sleep. PTSD fatigue is often more mental and emotional. |
| Trouble Concentrating | Yes | Yes | "Brain fog" from sleep apnea is often due to oxygen deprivation. In PTSD, it's more related to hypervigilance and intrusive thoughts. |
| Irritability/Mood Swings | Yes | Yes | With sleep apnea, irritability is a direct result of sleep deprivation. For PTSD, it's tied to emotional dysregulation and trauma triggers. |
| Waking Up Frequently | Yes | Yes | PTSD awakenings are often from nightmares or anxiety. Sleep apnea awakenings are the body's panic response to not breathing, often felt as gasping or choking. |
| Nightmares | Yes | No | Nightmares in PTSD are often replays of the traumatic event. This is a hallmark symptom not typically associated with sleep apnea itself. |
| Loud Snoring | No | Yes | Chronic, disruptive snoring is a classic sign of an obstructed airway, which is the core issue in sleep apnea. |
Recognizing these subtle differences is key. If you're experiencing symptoms from both columns—especially the unique hallmarks of each—it's a strong signal that you could be dealing with both conditions at once.
Why Integrated Treatment Is the Key to Recovery

Once you see the threads connecting PTSD and sleep apnea, it becomes obvious that you can't just treat one and ignore the other. Trying to work on trauma while a sleep disorder is wreaking havoc on your body is like trying to patch a leaky roof during a hurricane. It just doesn't work. True, lasting recovery requires tackling both problems at the same time.
This means if you have a PTSD diagnosis and your sleep is a mess, getting screened for sleep apnea should be high on your list. It usually starts with a simple conversation with your doctor, which can lead to a formal sleep study. And don't worry—it’s not as daunting as it sounds. Many of these studies can now be done right in the comfort of your own bed.
This study, officially called a polysomnogram, is designed to capture a complete picture of what happens when you sleep. It measures several key things:
- Brain Waves: To see exactly which sleep stages you're reaching (and which you're not).
- Heart Rate and Rhythm: To check for any strain on your cardiovascular system.
- Blood Oxygen Levels: To pinpoint the dangerous drops that happen when you stop breathing.
- Breathing Patterns: To count how many times per hour your breathing pauses or becomes shallow.
The data from the study gives doctors a clear diagnosis and shows just how severe the sleep apnea is, which is the first step toward getting the right help.
Creating a Collaborative Care Plan
For moderate to severe sleep apnea, the go-to treatment is Continuous Positive Airway Pressure, or CPAP therapy. A CPAP machine gently pushes air through a mask to keep your airway from collapsing while you sleep. Think of it as a small, steady air splint that prevents the cycle of choking, gasping, and waking up. The result? Deeper, more restorative rest.
But here’s the catch. For someone with PTSD, the idea of wearing a mask all night can be a huge hurdle. It can bring up feelings of being trapped or suffocated, making a difficult situation even worse. This is exactly why a one-size-fits-all approach fails.
When trauma is part of the picture, it's essential to bring in specialized support. This is where trauma-informed therapy makes a world of difference, as therapists can tailor their methods to create a sense of safety and control for the patient.
A collaborative care plan brings everyone to the same table—your sleep specialist, your therapist, and you. This team approach means that when you run into a problem, you have experts who can offer compassionate, practical solutions.
Integrated Treatment in Action: A sleep doctor might suggest trying a less intrusive nasal pillow mask. At the same time, your therapist could guide you through desensitization exercises, like wearing the mask for short, calm periods during the day to gradually build comfort and tolerance.
This kind of teamwork ensures that both your mind and body get the healing they need. The sleep specialist handles the mechanics of your breathing, while the therapist helps you navigate the psychological roadblocks. By addressing the issue from both sides, you create a powerful synergy that finally breaks the cycle and makes recovery a genuine reality.
Actionable Strategies for Better Sleep and Well-Being
When you're dealing with both PTSD and sleep apnea, there's no single magic bullet. It’s more about building a personal toolkit of strategies that support your mind and your body. Think of it as creating a system that puts you back in the driver's seat on your road to recovery.
For many, the first and most practical hurdle is simply getting comfortable with CPAP therapy. If you've experienced trauma, having a mask on your face can feel confining or even threatening. The key here is gradual desensitization. Don't force it. Just start by wearing the mask for short periods while you're awake and distracted—maybe while watching TV or listening to a podcast. This slowly helps your brain build a new, safer association with the mask, chipping away at the anxiety.
Creating a Secure Sleep Environment
Your bedroom needs to be your sanctuary. It should be a space that sends a clear signal to your brain: "you are safe here." This is absolutely critical for dialing down the hypervigilance that PTSD brings to the table, which can make the simple act of falling asleep feel like an impossible task.
Here are a few things you can do to make your bedroom a true haven:
- Minimize Triggers: Keep the room dark, quiet, and cool. Blackout curtains are fantastic for blocking out any sudden lights from outside, and a good sleep mask can do wonders.
- Establish a Calming Routine: An hour before bed, start winding down with relaxing activities. This could be reading a book (not on a bright screen!), doing some gentle stretching, or listening to calming music. This ritual helps your body and mind transition from a state of high alert to one of rest.
- Introduce Soothing Scents: Certain aromas, like lavender and chamomile, have been shown to promote a sense of calm. As one piece of your overall approach, you might find our guide to the 5 best essential oils for sleep apnea helpful in creating a more peaceful atmosphere.
A consistent, calming pre-sleep ritual does more than just relax you in the moment. It actually trains your nervous system to recognize that it's safe to power down, making it much easier to stick with your treatments night after night.
Building this solid foundation of sleep hygiene will amplify the benefits of any other treatments you're receiving. It’s all part of a bigger picture. As you move forward, you can also learn how to build healthy habits that actually stick, reinforcing all the positive changes you're making.
By taking these small, manageable steps, you create a powerful support system for yourself—one that leads to better sleep and, ultimately, a much brighter outlook.
Got Questions? We've Got Answers
When you're dealing with the complexities of PTSD and sleep apnea, a lot of questions come up. It's completely normal. Let's walk through some of the most common ones to give you a clearer picture.
If I Treat My Sleep Apnea, Will My PTSD Get Better?
It’s a resounding yes. When you effectively treat obstructive sleep apnea, often with CPAP therapy, it’s common to see a real improvement in PTSD symptoms. Think of it this way: deep, restorative sleep is when your brain does its heavy lifting—regulating emotions and processing trauma. Both conditions throw a wrench in that essential process.
By getting your sleep back on track and making sure your brain gets the oxygen it needs all night, CPAP therapy can dramatically cut down on daytime fatigue, lift your mood, and even make your trauma-focused therapies more effective. A mind that's truly rested is in a much better position to heal.
I'm a Veteran, but I Don't Have the Usual Risk Factors. Should I Still Get Tested?
Absolutely. While we often hear about risk factors like age and weight, the research is crystal clear: PTSD itself is a powerful, independent risk factor for sleep apnea, particularly for veterans. The relentless physiological stress that comes with PTSD can be enough to destabilize your airway all on its own.
Here's the bottom line: If you have PTSD and are struggling with things like crushing daytime sleepiness, loud snoring, or waking up feeling like you haven't slept at all, you should have a serious talk with your doctor about a sleep study. Don't let other risk factors hold you back.
The CPAP Mask Makes Me Feel Claustrophobic. What Can I Do?
This is a huge and very real hurdle for many people. The sensation of a CPAP mask can easily trigger feelings of being trapped, which is the last thing you need when dealing with PTSD. The key is to approach it with gradual desensitization.
Don't try to go from zero to eight hours overnight. Instead, take small steps to get comfortable with it.
- Start by just holding the mask.
- Next, try wearing it for short periods during the day while you're awake and doing something relaxing, like watching TV or listening to music.
- Work your way up to turning the machine on for a few minutes at a time.
You can also talk to your sleep specialist about different mask styles. Nasal pillows, for example, are much less intrusive than full-face masks. Pairing these practical steps with therapy to work through the anxiety is a proven strategy for making CPAP a sustainable part of your life.
At DubsLabs, we're focused on helping you create a sleep environment that feels safe and secure—a critical piece of the recovery puzzle. Our ultra-thin Bedphones and total-darkness sleep masks are designed to build a peaceful routine, making it easier to adapt to treatments and finally get the rest you deserve. Explore our collection of sleep solutions at DubsLabs.